Executive summary
This document considers the diagnosis of death by neurological criteria (DNC) in infants from 37 weeks corrected gestation (post menstrual) to two months (post term) of age.
Previous guidance has excluded infants in this age group due to the lack of evidence surrounding the presence of the required criteria for this group.
The working group reviewed the evidence published since the publication of the British Paediatric Association’s (BPA) report1 in 1991. After reviewing the evidence, the working group confirmed there is now sufficient evidence to extend the criteria for diagnosis in this patient population.
This guidance is provided for UK paediatric and neonatal health care staff working with infants under two months (post term) of age. This guidance is not applicable to pre term infants less than 37 weeks corrected gestation (post menstrual) age or infants older than two months post term. For infants older than two months the 2008 Academy of Medical Royal Colleges (AoMRC) A code of practice for the diagnosis and confirmation of death2 continues to apply.
After considering the relevant current evidence, these are the recommendations of the working group:
Preconditions
The working group recommends that the preconditions detailed in the 2008 AoMRC’s Code of Practice, and also expressed in the 1991 BPA report1, should be fulfilled before diagnosing DNC:
• The patient is comatose and mechanically ventilated for apnoea.
• The diagnosis of structural brain damage has been established or the immediate cause of coma is known (2008 AoMRC’s Code of Practice) and, in particular:
a. Drugs are not the cause of coma;
b. Neuromuscular blockade has been demonstrably reversed;
c. Hypothermia does not exist (temperature >34oC);
d. There is no endocrine or metabolic disturbance that could be the primary cause of the state of unresponsiveness.
The working group considered an extra precondition in this patient population was appropriate:
• In post-asphyxiated infants, or those receiving intensive care after resuscitation, whether or not they have undergone therapeutic hypothermia, there should be a period of at least 24 hours of observation during which the preconditions necessary for assessment for DNC should be present before clinical testing for DNC. If there are concerns about residual drug-induced sedation, then this period of observation may need to be extended.
Clinical diagnosis
The diagnosis of DNC using the clinical examination criteria used to establish death in adults, children and older infants, as outlined in the 2008 AoMRC’s Code of Practice2, can be confidently used for infants from 37 weeks corrected gestation (post menstrual) to two months post term:
• Absent brain stem reflexes
• Absent motor responses
• No respiratory response to hypercarbia
However in view of the immaturity of the newborn infant’s respiratory system, the following precautionary measure should be considered regarding the apnoea test:
• A stronger hypercarbic stimulus is used to establish respiratory unresponsiveness. Specifically, there should be a clear rise in the arterial blood partial pressure of carbon dioxide (PaCO2) levels of >2.7 kPa (>20 mm Hg) above a baseline of at least 5.3 kPa (40 mm Hg) to >8.0 kPa (60 mm Hg) with no respiratory response at that level.
The interval between tests need not be prolonged as stated in the 2008 AoMRC’s Code of Practice2.
Ancillary tests
Ancillary tests are not required to make a diagnosis of DNC in infants from 37 weeks corrected gestation (post menstrual) to two months post term.
1. Introduction
In 2008, The Academy of Medical Royal Colleges (AoMRC) published ‘A Code of Practice for the Diagnosis and Confirmation of Death’ and defined2 death as “the irreversible loss of those essential characteristics which are necessary to the existence of a living person and, thus, the definition of death should be regarded as the irreversible loss of the capacity for consciousness, combined with irreversible loss of the capacity to breathe.” [AoMRC’s Code of Practice, page 11].
In the 2008 Code of Practice2, the AoMRC took the position that death is a unitary state that might be reached following the cessation of cardiorespiratory function or in irreversible unresponsive coma with cessation of brain stem function. Detailed guidance was provided on the criteria for the diagnosis of death when it occurred after irreversible cardiorespiratory arrest (‘death by cardiac criteria’ (DCC)); or when it occurred in the course of unresponsive coma and in the absence of cardiorespiratory arrest (‘death by neurological criteria’ (DNC)). These terms are adopted in the present report. DNC may occur as a result of intracranial (for example, after traumatic head injury) or systemic events (for example, hypoxic-ischaemic injury).
In regard to the diagnosis of death in children, the 2008 AoMRC’s Code of Practice2 supported conclusions presented by the British Paediatric Association (BPA) (later to become the Royal College of Paediatrics and Child Health (RCPCH)) in a report published in 1991. The report stated: “over the age of two months, the criteria used to establish death should be the same as those in adults. Between thirty-seven weeks of gestation and two months of age, it is rarely possible to confidently diagnose death as a result of cessation of brain stem reflexes, and below thirty-seven weeks of gestation the criteria to establish this cannot be applied” [2008 AoMRC’s Code of Practice, page 18].
Following this recommendation, neonatal teams in the UK currently do not diagnose DNC in young infants. However, other countries3-5 around the world do accept determination of death in young infants by certain neurological criteria in the presence of persisting cardiac function.
1.1 Scope and objectives of the report
This report is an update of the 1991 BPA report1 which is included as an appendix in the 2008 AoMRC’s Code of Practice2. It aims to take account of contributions to evidence in the medical literature from 1990 to 2014 relating to the diagnosis of death in young infants from 37 weeks corrected gestation (post menstrual) to two months post term. This report does not cover broader issues around withdrawal or withholding medical treatment in children which are covered in the RCPCH 2015 Ethics Advisory Committee report6 or issues surrounding organ donation and transplantation.
This report sets out to address the following three questions in regard to infants born 37 weeks corrected gestation (post menstrual) to two months post term:
1. Can the clinical criteria used to diagnose DNC in older infants, children and adults be applied to these young infants?
2. Should there be preconditions for the diagnosis of DNC in these young infants that are additional to those applied to older infants, children and adults?
3. Can ancillary tests provide us with additional relevant information in the diagnosis of DNC?
1.2 Target audience
This report is intended for use by all UK paediatric and neonatal health care practitioners and other groups involved in the regulation or practice of the health care of critically ill neonates and young infants.
1.3 Target population
This report addresses the diagnosis of DNC in infants between the ages of 37 weeks corrected gestation (post menstrual) and two months post term.
1.4 Exclusions
This report does not include recommendations for the management of pre term infants, below 37 weeks gestation.
2. Methodology
This report has been developed in accordance with the RCPCH Standards for Development of Clinical Guidelines in Paediatrics and Child Health which has National Institute for Health and Care Excellence (NICE) accreditation. A systematic review was carried out and the process to develop the guidance included the development of relevant clinical questions, systematic search of the literature in electronic databases, selection of the evidence according to predetermined inclusion criteria, critical appraisal of the included papers and assessment of the evidence using the Scottish Intercollegiate Guideline Network (SIGN) grading hierarchy. In instances where there was no strong evidence to be found, recommendations were agreed by working group consensus.
An assessment was also carried out on the degree of detail reported in each study regarding the diagnosis of death in the presence of persisting cardiac function. Studies were categorised as I, II or III depending on which clinical features were described (see Table 1 for more details).
Table 1. Degree of information given in studies of diagnosis of death in the presence of persisting cardiac function in infants under two months.
| Degree of detail | Clinical features of death in the presence of persisting cardiac function described in the report |
|---|---|
| I | Coma; brain stem reflexes individually described; reflex respiratory response to hypercarbia formally tested (the apnoea test). |
| II | As for degree I, but brain stem reflexes not individually reported. |
| III | Death in the presence of persisting cardiac function reported, but individual clinical features not described in any detail. |
3. Clinical diagnosis of death by neurological criteria
Question 1: Can the clinical criteria used to diagnose DNC in older infants, children and adults be applied to young infants?
In the 2008 AoMRC’s Code of Practice2 the clinical diagnosis of DNC rested on two elements; the identification of irreversible loss of consciousness and the absence of brain stem reflexes, including an apnoea test.
In regard to infants, coma can be recognised in those aged less than two months. Unresponsive coma is not uncommon in infants secondary to birth trauma and perinatal asphyxia, and it is also seen in the first few months of life following apparent life threatening events and head trauma from accidents or inflicted injury. Unresponsiveness can be evaluated and expressed on a coma scale in such infants in the same way as older infants and children.
The reflexes for brain stem function include:
• Pupillary response to light
• Corneal reflex
• Vestibulo-ocular reflex (Caloric test)iv
• Motor response to pain in the distribution of cranial nerve V (i.e. facial grimace or other motor response to supra-orbital pressure)
• Gag and cough reflex in response to oropharyngeal stimulation and suction through an endotracheal tube or tracheostomy
• Respiratory response to rise in arterial blood partial pressure of carbon dioxide (PaCO2)
3.1 Evidence review
The literature was searched from 1990 to 2014 for cases of infants whose death was diagnosed from 37 weeks corrected gestation (post menstrual) to two months post term. Thirteen studies [SIGN level of evidence 3] were identified in the literature and are summarized in Appendices 1.1 to 1.3.
3.1.1 Clinical examination
Thirteen studies were identified describing 42 infants younger than two months whose diagnosis of death was determined by certain neurological criteria despite persisting cardiac function and where sufficient detail is provided to support this diagnosis (see Appendix 1.1 for a summary of the studies). In the 42 cases identified from 13 studies, the degree of detail describing the cases was I in six studies , II in six studies, and III in one study21 (see Table 1 for more information about the different degrees of detail). Thus the brain stem reflexes were individually described in 27 infants, in six studies (degree of detail I)9-14, and in 14 infants in six studies (degree of detail II)15-20 the majority of brain stem reflexes were described (although not all were individually reported).
The diagnostic guidance used in each of the 13 studies is summarized in Appendix 1.2. One major difference between the national guidelines is whether electroencephalography (EEG) should be used as part of the diagnosis of death in the presence of persisting cardiac function. Its use was included in 10 of the 13 studies. The use of EEG is considered in Section 5.
3.1.2 Apnoea test
Twelve of the studies identified described the criteria used in the apnoea test. In 10 of these studies the national guidelines required a minimum PaCO2 to test respiratory response to hypercarbia of 8.0 kPa (60 mm Hg). In fact, the PaCO2 achieved during the apnoea test varied from 6.9 to 19.1 kPa. The other two studies used the 1987 national guidelines from Canada (see Parker10 for reference details) and the 1991 BPA report,1 in which the minimum level in PaCO2, to determine respiratory unresponsiveness, was 6.7 kPa (50 mm Hg).
3.1.3 Duration of interval between tests
All of the studies in Appendices 1.1 to 1.3 used two examinations in order to declare death. The interval between the first and second examinations is described in 11 studies; ranging from 30 minutes to four days or greater.
3.1.4 Duration of interval after second examination and cessation of cardiac function
The interval between the second examination for the diagnosis of death in the presence of persisting cardiac function and discontinuation of supportive mechanical ventilation was only reported in some of the studies9-16,19-21 and ranged from a few hours to three weeks; seven infants had respiratory support continued for a week or more (see Appendix 1.3 for a summary of the cases). There were no cases identified where supportive treatment was continued until cardiac arrest. None of the infants in these studies regained brain stem function, breathing, or consciousness during the period of observation.
3.2 Working group interpretation
In the 42 cases identified in the evidence, no infants regained brain stem function after meeting neurological criteria. Although this evidence is limited to case reports and case series [SIGN level of evidence 3], there is now a reasonable body of international medical literature that describes the determination of death by certain neurological criteria in the presence of persisting cardiac function in infants from 37 weeks corrected gestation (post menstrual) to two months post term. Twelve studies described in detail (degree I and II, see Table 1 for description of degree of detail) the assessment of brain stem reflexes, similar to the detail required for the diagnosis of DNC as recommended in the 2008 AoMRC’s Code of Practice.
The working group could find no developmental or other rationale for the specification of a higher threshold level of hypercarbia to that stated in the 1991 BPA1 and 2008 AoMRC2 reports to demonstrate respiratory unresponsiveness but noted that reports of death in younger infants in the presence of persisting cardiac function have used higher minimum levels than are routinely used in older infants and children.
In regard to the repetition of testing, most studies in the literature have reported intervals between clinical testing longer than the “short period of time” prescribed in the 2008 AoMRC’s Code of Practice. The working group supports the view of the BPA1 and AoMRC2 reports that the prime purpose of the second examination is to minimize the possibility of an incorrect diagnosis because of error in the first examination. The working group could find no cogent rationale for specifying a precise interval between clinical examinations. Instead, the view of the working group was that an appropriate period of observation and assessment of preconditions before testing for DNC should be specified.
As a result of reviewing the evidence and international guidance the working group concluded that the diagnosis of DNC using the clinical examination criteria used to establish death in adults, as outlined in 2008 AoMRC’s Code of Practice can be diagnosed confidently in young infants using the same criteria as for older infants. However in view of the importance of maximum safeguarding of the security of the diagnosis of DNC in these very young infants, the working group concluded that a longer period of observation prior to testing and a higher level of PaCO2 compared to the criteria described in the AoMRC’s Code of Practice for the apnoea test should be adopted at the present time.
4. Preconditions
Question 2: Should there be preconditions for the diagnosis of DNC in young infants that are additional to those applied to older infants, children and adults?
The 2008 AoMRC and 1991 BPA reports specify a number of conditions that must be fulfilled before the diagnosis of DNC following irreversible cessation of brain stem function can be undertaken, including:
• Aetiology of irreversible brain damage: There should be no doubt that the patient’s condition is due to irreversible brain damage of known aetiology;
• Exclusion of potentially reversible causes of coma: The patient is deeply comatose, unresponsive and apnoeic, with his/her lungs being artificially ventilated;
o There should be no evidence that this state is due to depressant drugs: If there is any doubt about the action of narcotics, hypnotics and tranquillizers (particularly when hypothermia coexists or in the presence of renal or hepatic failure) then specific drug levels should be measured and shown to be within or below therapeutic range, before proceeding;
o Primary hypothermia as the cause of unconsciousness must have been excluded: The core temperature should be greater than 34oC at the time of testing;
o Potentially reversible circulatory, metabolic and endocrine disturbances must have been excluded as the cause of the continuing unconsciousness;
• Exclusion of potentially reversible causes of apnoea: Neuromuscular blocking agents and other drugs must have been excluded as the cause of respiratory inadequacy or failure. In addition, the presence of cervical cord injury must be excluded in infants where trauma is the mechanism of coma. [2008 AoMRC’s Code of Practice, page 14-16]
4.1 Evidence review
The selected studies described in Section 3 (Appendix 1.1) were reviewed with the purpose of making recommendations with regard to preconditions for the determination of death in the presence of persisting cardiac function. In each of the 13 studies (see Appendix 1.1 for a summary of the cases), the guidelines used the following preconditions:
• The aetiology of the irreversible brain problem should be known.
• Potentially reversible causes of coma should have been excluded.
• Potentially reversible causes of apnoea should have been excluded.
The literature search did not retrieve any additional evidence on the subject of preconditions.
4.2 Working group interpretation
The working group reviewed the retrieved evidence, the international guidelines used in the evidence (see Appendix 1.2 for a summary), along with the 2008 AoMRC and 1991 BPA1 reports, and considered that there was insufficient information to justify the use of different preconditions for diagnosis of DNC in infants aged 37 weeks corrected gestation to two months post term. The working group considered that the particular context in which the question of DNC arises in this age group will commonly include hypoxic-ischaemic injury and/or recent birth before which the infant cannot have been directly observed. Therefore, a period of observation after birth is required in order to confirm irreversibility of unresponsiveness is a reasonable additional precautionary measure in this age group.
There was no evidence found to guide the diagnosis of DNC in infants who have undergone therapeutic hypothermia. However, the working group considered that such treatment (to a temperature of 33.5oC) was an important issue for the diagnosis of DNC in newborn infants. Therapeutic hypothermia has recently been adopted as a standard of care for infants with hypoxic-ischaemic encephalopathy, and its use may influence the clinical assessment of DNC. The working group also raised concerns that this treatment may impair clearance of opiates, benzodiazepines and barbiturates used for comfort.
The working group concluded that it was important to include these preconditions for the diagnosis of DNC in infants aged 37 weeks corrected gestation to two months post term. The recommendations included in this report are likely to bring about a change in practice, and the working group concluded that it was necessary to be cautious in the clinical assessment and diagnosis of DNC for this reason.
5. The use of ancillary tests in the diagnosis of death by neurological criteria
Question 3: Can ancillary tests provide us with additional relevant information in the diagnosis of DNC?
In the 2008 AoMRC’s Code of Practice, ancillary tests are not required to establish the diagnosis of DNC and they should not be used as a substitute for the neurological examination. However, death cannot be diagnosed by the testing of brain stem reflexes alone in instances where a comprehensive neurological examination is not possible, for example:
a) “When there is uncertainty about the results of the clinical examination such as occurs with extensive facio-maxillary injuries, or in cases of high cervical cord injury, or in cases with residual sedation;
b) When the apnoea test cannot be completed because the medical condition of the patient results in the development of hypoxia or hypotension during the testing;
c) When the effect of a primary metabolic or pharmacological derangement cannot be ruled out”.
The ancillary tests that have been reported in previous findings for infants include:
• Clinical Neurophysiology: EEG, evoked potentials (somatosensory or brain stem auditory).
• Cerebral blood flow: transcranial Doppler ultrasound, computed tomography with injection of contrast material or Xenon inhalation, digital subtraction angiography, single photon positron emission computed tomography (SPECT), and positron emission tomography (PET).
Many of these tests rely on assessing some threshold of activity, above which values are accepted as satisfactory and below which they are not. However, thresholds for detection of any such activity do not necessarily indicate, or guarantee, the presence of adequate function in the infant brain. Some function can occur below the activity threshold level and in some cases there may be negligible function despite demonstrable activity above threshold.
5.1 Evidence review
The working group initially searched the literature for published cases of patients where death was diagnosed in infants from 37 weeks corrected gestation to two months post term, and where ancillary tests were used to inform the diagnosis. Due to the lack of evidence identified, the inclusion criterion was widened to include infants up to 12 months of age, to determine the reliability of ancillary tests.
All publications were case series and case reports [SIGN level of evidence 3]. The summary data in Appendix 1.4 indicate that ancillary investigations do not aid the bedside determination of death in the presence of persisting cardiac function. EEG is the most widely available ancillary test in most clinical centres caring for critically ill infants (see Appendix 1.2 and 1.4 for summaries); often with the criteria of death in the presence of persisting cardiac function including the finding of isoelectric EEG on two occasions. However, absent electrical activity is not judged necessary for a diagnosis of DNC in the 2008 AoMRC’s Code of Practice. Also, an isoelectric EEG was not required as part of guidelines from Germany (1991)15, Canada (1987)10 and the UK (1991)13, as shown in Appendix 1.2.
The studies showed instances of false negatives and false positives when using EEG along with clinical criteria for the determination of death with persisting cardiac function. The literature search identified 11 studies10,15-17,23-29 that described the use of EEG to aid the diagnosis of “brain death”. One study found three out of 17 infants who met “brain death” criteria had electrocerebral silence (ECS)10; another found EEG activity in 15 of 29 children at the time these patients met national (Spain) “brain death” clinical criteria. There are other such reports of infants under one year of age.
Similar instances of false negatives and false positives were reported when using tests of cerebral blood flow.
5.2 Working group interpretation
The review of the evidence suggests that all of the investigations used as ancillary tests in the diagnosis of DNC in adults and children could be inaccurate when applied to young infants. Such investigations do not aid the clinical assessment of DNC in young infants.
Therefore, the working group considered that if reliable clinical assessment is not possible because of residual sedation, primary metabolic or pharmacological derangement, then assessment should be made when these confounding factors are no longer present. In infants where there is uncertainty about the results of the clinical examination (e.g. extensive facio-maxillary injuries, or high cervical cord injury, or inability to perform the apnoea test), the limitations of using ancillary tests should be recognised and should not be used to assist diagnosis. Since the diagnosis of DNC does not denote cessation of all neurological activity in the brain, but the irreversible loss of the capacity for consciousness combined with the cessation of brain stem function as determined by the clinical testing described in Section 3, ancillary tests that demonstrate some neurological activity do not invalidate a clinical diagnosis of DNC.
6. Recommendations on the diagnosis of DNC
Preconditions
The working group recommends that the preconditions detailed in the 2008 AoMRC’s Code of Practice, also expressed (in less detail) in the 1991 BPA report1, should be fulfilled before diagnosing DNC:
• “The patient is comatose and mechanically ventilated for apnoea (2008 AoMRC’s Code of Practice).
• The diagnosis of structural brain damage has been established or the immediate cause of coma is known (2008 AoMRC’s Code of Practice) and, in particular:
– Drugs are not the cause of coma;
– Neuromuscular blockade has been demonstrably reversed;
– Hypothermia does not exist (temperature >34oC);
– There is no endocrine or metabolic disturbance that could be the primary cause of the state of unresponsiveness”.
An additional precautionary precondition to be taken in young infants:
• In post-asphyxiated infants, or those receiving intensive care after resuscitation, whether or not they have undergone therapeutic hypothermia, there should be a period of at least 24 hours of observation during which the preconditions necessary for assessment for DNC should be present before clinical testing for DNC. If there are concerns about residual drug-induced sedation, then this period of observation may need to be extended [Level 3, Grade D].
Clinical diagnosis of DNC
The diagnosis of DNC using the clinical examination criteria used to establish death in adults, children and older infants, as outlined in the 2008 AoMRC’s Code of Practice, can be confidently used in infants from 37 weeks corrected gestation (post menstrual) to two months post term [Level 3, Grade D].
The following precautionary measures should be considered:
• A stronger hypercarbic stimulus is used to establish respiratory unresponsiveness. Specifically, there should be a clear rise in PaCO2 levels of >2.7 kPa (>20 mm Hg) above a baseline of at least 5.3 kPa (40 mm Hg) to >8.0 kPa (60 mm Hg) with no respiratory response at that level [Level 3, Grade D].
• The interval between tests need not be prolonged as stated in 2008 AoMRC’s Code of Practice.
Ancillary tests
Ancillary tests are not required to make a diagnosis of DNC in infants from 37 weeks corrected gestation (post menstrual) to two months post term [Level 3, Grade D].
In cases where a clinical diagnosis of DNC is not possible (for example because of extensive facio-maxillary injuries, or high cervical cord injury), ancillary tests are not sufficiently robust to help confidently diagnose DNC in infants [Level 3, Grade D].
6.1 Procedure for the diagnosis and confirmation of cessation of brain stem function (Guide)
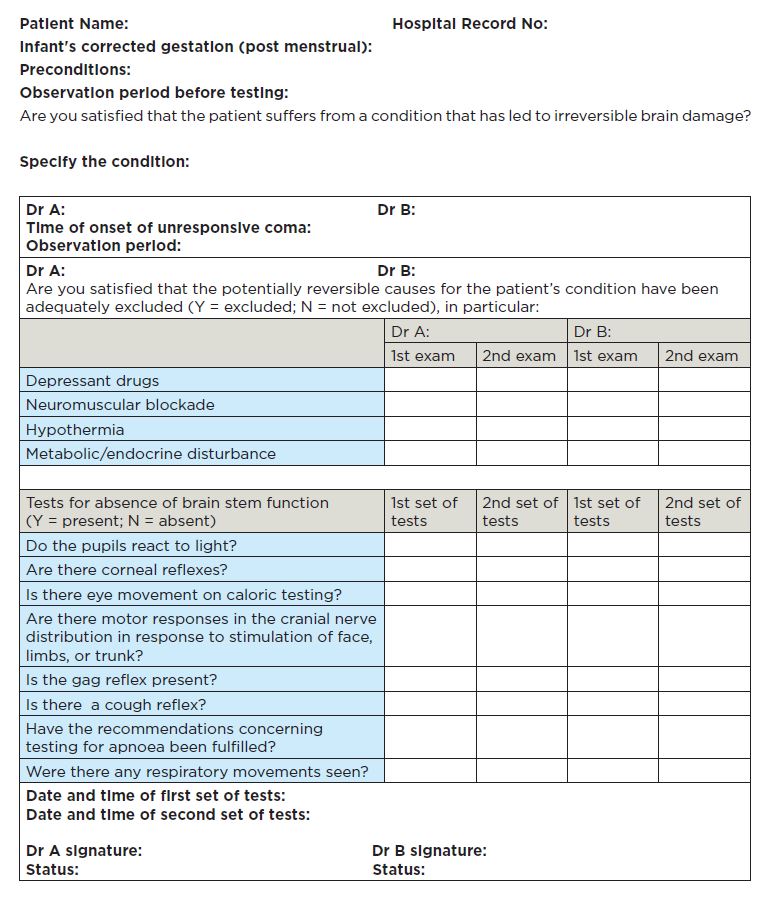
Click here to download the editable PDF version
6.2 Diagnostic and management algorithm
Identification of coma
Clinical evidence of cause of coma with likely mechanism leading to death by neurological criteria (DNC)
(possibly supported by history, neuroimaging, cerebrospinal fluid, etc.)
Yes
Exclusion of
• Hypothermia
• Intoxication
• Sedative drugs
• Neuromuscular blocking agents
• Severe electrolyte, acid-base or endocrine abnormality
Absent brain stem reflexes
Absent motor responses
Apnoea with clear rise in PaCO2 levels of >2.7 kPa (>20 mm Hg) above a baseline
of at least 5.3 kPa (40 mm Hg) to >8.0 kPa (60 mm Hg)
These procedures should be clearly explained to relatives and carers

Yes

Clinical diagnosis of death by neurological criteria
Click here to download the PDF version
7. Implications for practice
7.1 Guideline update
It is recommended that the guidance in this report is updated so that clinical recommendations take into account important new information. The evidence should be reviewed five years after publication, and the views of health care professionals, parents and carers should be sought to assess whether the guidance requires updating. If new evidence is published between updates it may be decided that a more rapid update of some of the recommendations is necessary.
7.2 Research recommendations
• A study to define more clearly the developmental trajectory of brain stem reflexes in pre term infants.
• A British Paediatric Surveillance Unit study should be carried out to assess the impact of widening the age range in which a diagnosis of DNC is made to include the period of 37 weeks corrected gestation (post menstrual) to two months post term.
• A study to incorporate the views of parents of infant whose death is established in this way and of health care professionals involved in the process of diagnosing DNC (i.e. nurses and medical staff). This should include ascertainment at both a short and a longer interval after the event.
7.3 Editorial independence
The report update was internally funded by the RCPCH and all working group members declared all conflicts of interests, which were recorded
7.4 Implementation
The report is available on the RCPCH website (Clinical Guidelines and Standards section). In addition, all confirmed stakeholders will be approached for direct publication on their website or via a link to the RCPCH site.
7.5 Implementation advice
Clinicians working in intensive care are highly skilled at supporting parents and carers at the time of the death of their infant and have developed a range of practices relating to withdrawal of treatment6. Parents have been shown to be appreciative of sensitive bereavement support and care. Bereavement can be difficult and demanding for those working with infants and families around the time of death. When a diagnosis of DNC occurs, new challenges may arise for clinicians as well as for parents, and current practices of bereavement support may need to evolve in response.
A diagnosis of DNC may require some degree of extension to the observation period prior to the first clinical test for DNC. The implications of this for parents are not yet known. Such a delay may or may not be problematic. When the dying process is extended, for instance by a lingering death after withdrawal of treatment, this is known to be a potential cause of parental distress especially if there is a mismatch of expectations and events. A quick death after redirection of care has been shown to be seen as an affirmation of the decision that was made, while a lingering death can raise parental doubts. In the situation considered in this report the timescale of the assessment process and any signs which may suggest hope may be difficult for parents and may complicate their experience and subsequent bereavement. It may be the case that additional time that is expected and planned for, and the careful accumulation of evidence to inform and support a decision may be viewed positively by parents and by clinicians.
7.6 Resource implications
Following the recommendations stated in this report, the need for ongoing training and support might have financial implications, particularly for smaller units. Physicians will need training in the diagnosis of DNC in young infants from 37 weeks corrected gestation (post menstrual) to two months post term, and all health care practitioners will need training in managing bereavement when this diagnosis is made. Neonatal paediatricians are unlikely to have experience of making the diagnosis of DNC and will require close liaison with paediatric neurologists and intensivists locally when making a diagnosis. The 2008 AoMRC’s Code of Practice states:
(The) diagnosis should be made by two doctors who have been registered for more than five years and are competent in the procedure. At least one should be a consultant. Testing should be undertaken by the doctors together and must always be performed completely and successfully on two occasions in total.” (2008 AoMRC’s Code of Practice, page 22).
Paediatricians making the diagnosis of DNC should meet these criteria.
The recommendations in this report might present challenges for clinicians emotionally and ethically. Clinicians and health care teams should provide support to parents and carers of infants being clinically assessed for DNC, to ensure they are well informed and have access to any emotional support they require. Training should be available for paediatricians to offer bereavement support and, where appropriate, direct families to those who can provide further advice and information. Clear, easy-to-understand information should be provided to parents and carers at all stages. It will be important that parents have access to clear information to help them understand the determination of DNC, and health care professionals will need to provide supportive care to help them incorporate this information into their understanding of the processes surrounding their infant’s death.
8. Glossary
| 8.1 Definitions | |
| Coma | A state of unconsciousness lasting for six hours or more. |
| Corrected gestation | The gestational age that the baby was born at plus the number of completed weeks after birth. |
| Cerebral blood flow (CBF) | The volume of blood flowing through the brain in a particular time. The units are mL/100 gm brain tissue/minute. |
| Death by cardiac criteria (DCC) | The consequence of irreversible loss of cardiac function, with cardiac arrest. |
| Death by neurological criteria (DNC) | The irreversible loss of those essential characteristics which are necessary to the existence of a living person (loss of the capacity for consciousness, combined with loss of the capacity to breathe) |
| Electrocerebral silence (ECS) | Electrocerebral silence as determined by EEG recording, showing absence of electrical activity in the brain. Also known as an isoelectric electroencephalogram (EEG). |
| Transcranial doppler (TCD) | TCD is a technique used to measure the velocity of blood in the cerebral blood vessels. |
| 8.2 Abbreviations | |
| AAP | American Academy of Pediatrics |
| AoMRC | Academy of Medical Royal Colleges |
| BPA | British Paediatric Association (forerunner of the Royal College of Paediatrics and Child Health) |
| CBF | Cerebral blood flow |
| CO2 | Carbon dioxide |
| DCC | Death by cardiac criteria |
| DNC | Death by neurological criteria |
| ECS | Electrocerebral silence |
| EEG | Electroencephalography |
| O2 | Oxygen |
| PaCO2 | Partial pressure of carbon dioxide in arterial blood |
| PaO2 | Partial pressure of oxygen in arterial blood |
| PET | Positron emission tomography |
| RCPCH | Royal College of Paediatrics and Child Health |
| SPECT | Single photon positron emission computed tomography |
| TCD | Transcranial Doppler |
